- Chi tiết
-
Được đăng: 02 Tháng 3 2016
Abstract
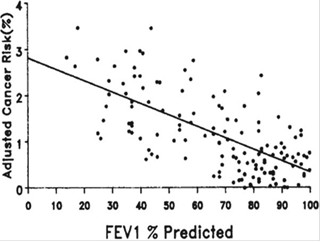
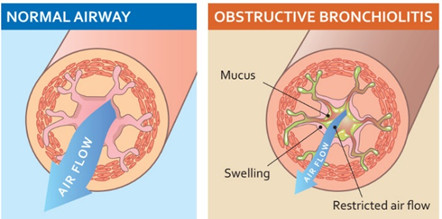
The diagnostic criteria of asthma–chronic obstructive pulmonary disease (COPD) overlap syndrome (ACOS) advocated by the Global Initiative for Asthma (GINA)/Global Initiative for Chronic Obstructive Lung Disease (GOLD) are somewhat complicated, and limited data are available regarding how ACOS patients respond to current medications. We present a case of a 64-year-old man with ACOS. With features favoring asthma including childhood asthma history with intermittent episodes of dyspnea at night, elevated blood eosinophil count and total IgE, increased forced expiratory volume in 1 s (FEV 1 ) after bronchodila-tor (>200 mL and >12% from baseline), and positive skin prick tests, he also had features favoring COPD such as heavy smoker, persistent exertional dyspnea, and airflow limitation after inhaled therapy. Over 5-year follow up, our patient experienced a single episode of moderate exacerbation. However, post-bronchodilator FEV 1 decreased by 240 mL for 4 years (−60 mL/year) after 1.5 years of treatment, indicating rapid lung function decline. Longitudinal studies are necessary to assess optimal interventions and natural course of ACOS.